

Users may view institutional claims, which contains 12 data entry tabs.
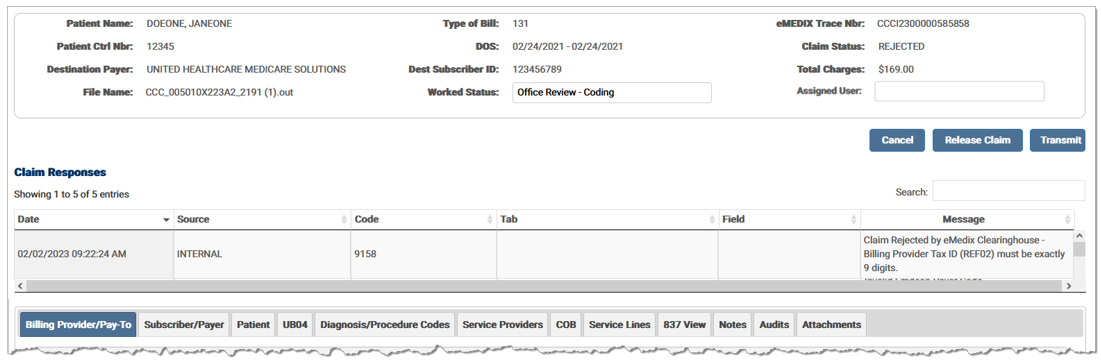
The Billing Provider/Pay-To tab contains Billing and Pay-To claim data.
The Subscriber/Payer tab contains information about the insurer and insured person. It includes Primary, Secondary, and Tertiary options for the Payer and the Subscriber. A claim must have at least one payer and subscriber.
The Patient tab contains patient specific information, including demographic information.
The UB04 tab contains information regarding data sent from the Hospital I/S files. Options are located within accordion banners. Click the desired banner and enter any information needed for the claim.
The Diagnosis/Procedure Codes tab supplies information related to the delivery of health care. Principal diagnosis information displays when the tab is selected. Other options are located within accordion banners. Click the banner to display the associated fields.
The Service Providers tab contains information regarding the various claim level service providers. Enter any information on the Rendering Provider, Referring Provider, Additional Referring Provider Information, Supervising Provider, and/or Service Facility Provider.
The claim level Coordination of Benefits information is entered in the COB tab. This information is used to indicate the total monetary amount reported.
The Service Lines tab contains the procedures and charges for the claim or encounter.
The 837 View tab contains the current claim data in an ANSI format.
The Audits tab contains a record of changes made to the claim.
The Notes tab contains any notes associated with the claim and allows users to attach notes to the claim.
The Attachments tab contains information regarding attachments for the claim. Users can upload and submit attachments to payers. This tab is only visible if the payer accepts electronic or print/mail attachments.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.