

The claim level Coordination of Benefits (COB) information displays here. This information is used to indicate the total monetary amount reported. When a user enters the Payer Name in the payer section, the name displays on the accordion banner for each payer type (primary, secondary, tertiary).
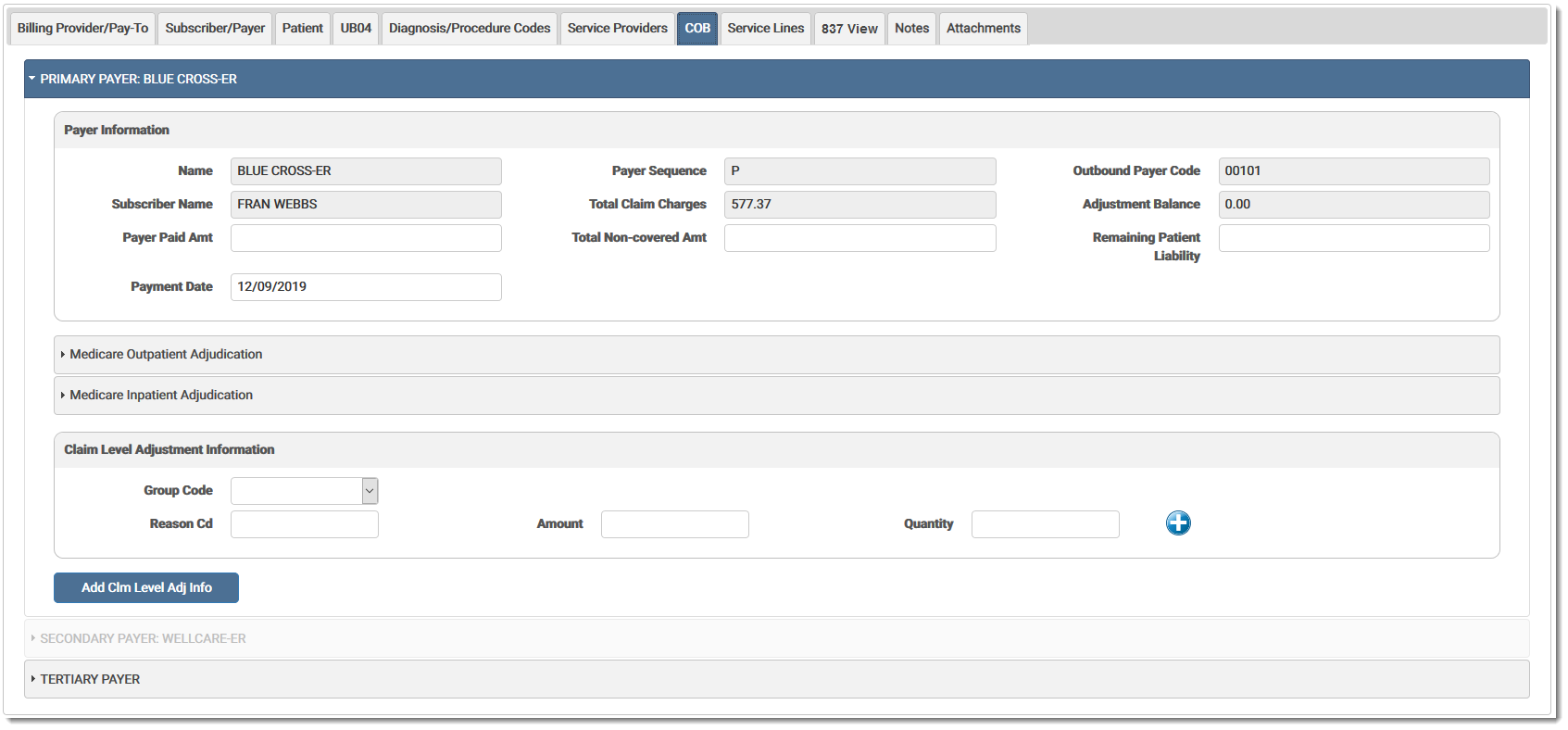
The COB fields are defined below (gray fields are disabled):
Patient Information (Primary, Secondary, and Tertiary Payer)
The Health Plan responsible for payment.
The order in which the Health Plan is responsible for payment - first, second, or third, usually labeled primary, secondary, or tertiary.
Outbound Payer CodeOutbound Payer Code
The payer code which identifies the Destination Health Plan. If the inbound payer code is not valid, eMEDIX will route to the correct outbound payer code.
Subscriber NameSubscriber Name
The person identified as the holder of the Health Plan policy.
Total Claim ChargesTotal Claim Charges
The total of all procedures charged on the claim.
Adjustment BalanceAdjustment Balance
The sum of all the adjustments.
Payer Paid AmountPayer Paid Amount
Dollar amount paid by the provider.
Total Non-Covered AmountTotal Non-Covered Amount
Dollar amount not covered by the payer and excluded for payment.
Remaining Patient Liability Remaining Patient Liability
Dollar amount that the patient is responsible to pay after all the payers have paid.
The date of the payment by the Health Plan.
Claim Level Adjustment Information
Code identifying the general category of payment adjustment. Options are:
| CO | Contractual Obligations |
| CR | Correction and Reversals |
| OA | Other Adjustments |
| PI | Payer Initiated Reductions |
| PR | Patient Responsibility |
Code Identifying the detailed reason for the adjustment. Up to six (6) reason codes can be added.
The amount of the adjustment.
The unit of service being adjusted. Required when the number of service units has been adjusted.
Add Claim Level Adjustment InformationAdd Claim Level Adjustment Information (button)
Click to add another claim level adjustment. Up to five (5) adjustments can be added.
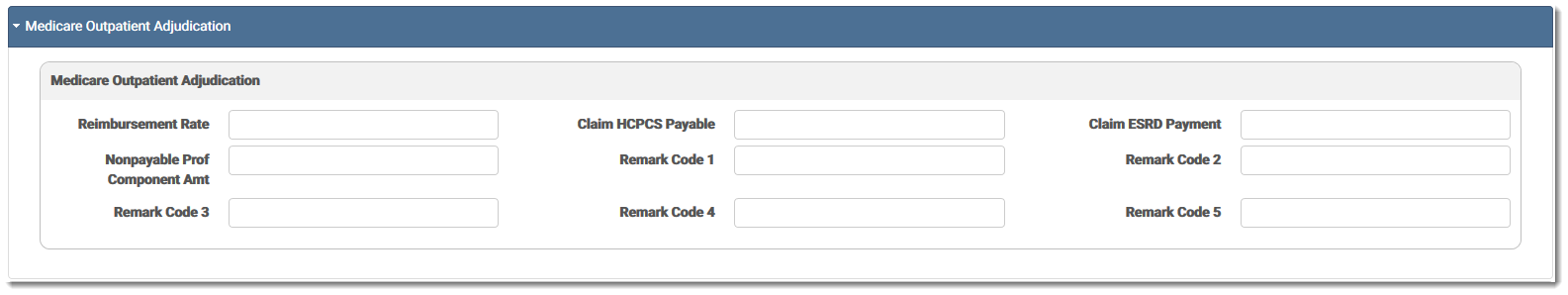
Medicare Outpatient Adjudication
Reimbursement RateReimbursement Rate
Reimbursement rate percentage expressed as a decimal. Required when returned in the remittance advice.
Claim HCPCS PayableClaim HCPCS Payable
The claim Health Care Financing Administration Common Procedural Coding System (HCPCS) payable amount. Required when returned in the remittance advice.
Claim ESRD PaymentClaim ESRD Payment
The End State Renal Disease (ESRD) payment amount. Required when returned in the remittance advice.
Non-Payable Prof Component AmountNon-Payable Prof Component Amount
The professional component amount billed but not payable. Required when returned in the remittance advice.
Remark Codes 1-5Remark Codes 1-5
Used to provide additional explanation for an adjustment already described by a Claim Adjustment Reason Code (CARC), or to convey information about remittance processing.
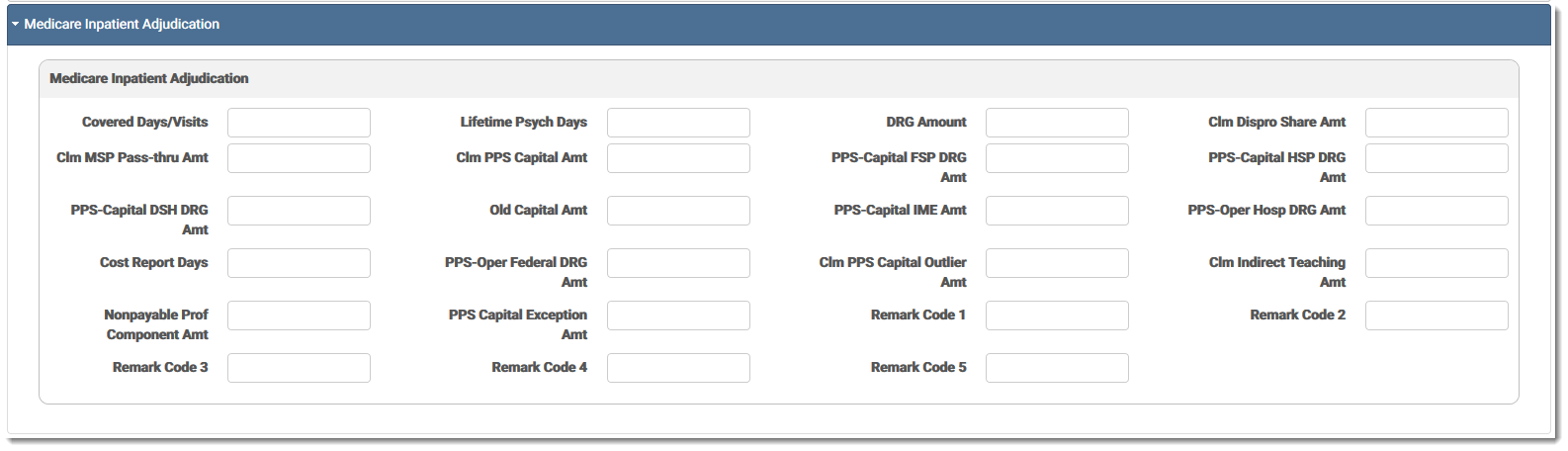
Medicare Inpatient Adjudication
Covered Days/VisitsCovered Days/Visits
The quantity of inpatient days or visits covered by Medicare.
Lifetime Psych DaysLifetime Psych Days
The quantity of inpatient lifetime psychiatric days covered by Medicare.
The dollar value of the Diagnosis Related Group (DRG) amount on this claim.
Claim Dispro Share AmountClaim Dispro Share Amount
Dollar value of the disproportionate share amount on this claim.
Claim MSP Pass-Thru AmountClaim MSP Pass-Thru Amount
Dollar value of the Medicare Secondary Payer (MSP) pass-through amount on this claim.
Claim PPS Capital AmountClaim PPS Capital Amount
Dollar value of the total Prospective Payment System (PPS) capital amount on this claim.
PPS-Capital FSP DRG AmountPPS-Capital FSP DRG Amount
Dollar value of the Prospective Payment System (PPS) capital, federal-specific portion, Diagnostic Related Group (DRG) amount.
PPS-Capital HSP DRG AmountPPS-Capital HSP DRG Amount
Dollar value of the Prospective Payment System (PPS) capital, hospital-specific portion, Diagnosis Related Group (DRG) amount.
PPS-Capital DSH DRG AmountPPS-Capital DSH DRG Amount
Dollar value of the Prospective Payment System (PPS) capital, disproportionate share, hospital Diagnosis Related Group (DRG) amount.
Old Capital AmountOld Capital Amount
Dollar value of the old capital amount.
PPS-Capital IME AmountPPS-Capital IME Amount
Dollar value of the Prospective Payment System (PPS) capital Indirect Medical Education (IME) claim amount.
PPS-Oper Hospital DRG AmountPPS-Oper Hospital DRG Amount
Dollar value of the hospital-specific Diagnosis Related Group (DRG) amount.
Cost Report DaysCost Report Days
The quantity of Medicare inpatient cost report days.
PPS-Oper Federal DRG AmountPPS-Oper Federal DRG Amount
Dollar value of the federal-specific Diagnosis Related Group (DRG) amount.
Claim PPS Capital Outlier AmountClaim PPS Capital Outlier Amount
Dollar value of the Prospective Payment System (PPS) capital outlier amount on this claim.
Claim Indirect Teaching AmountClaim Indirect Teaching Amount
Dollar amount of the indirect teaching amount on this claim.
Non-Payable Prof Component AmountNon-Payable Prof Component Amount
The professional component amount billed but not payable. Required when returned in the remittance advice.
PPS-Capital Exception AmountPPS-Capital Exception Amount
Dollar value of the PPS capital exception amount.
Used to provide additional explanation for an adjustment already described by a Claim Adjustment Reason Code (CARC), or to convey information about remittance processing.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.