

The Destination Payer Information displays in this section. The data is not editable. The destination payer information is pulled into RCM from the claim. If a user wants to change the destination payer, they may do so by changing the File Claim To in the drop-down menu. If the provider changes the destination payer to sequence with no payer, an error message displays.
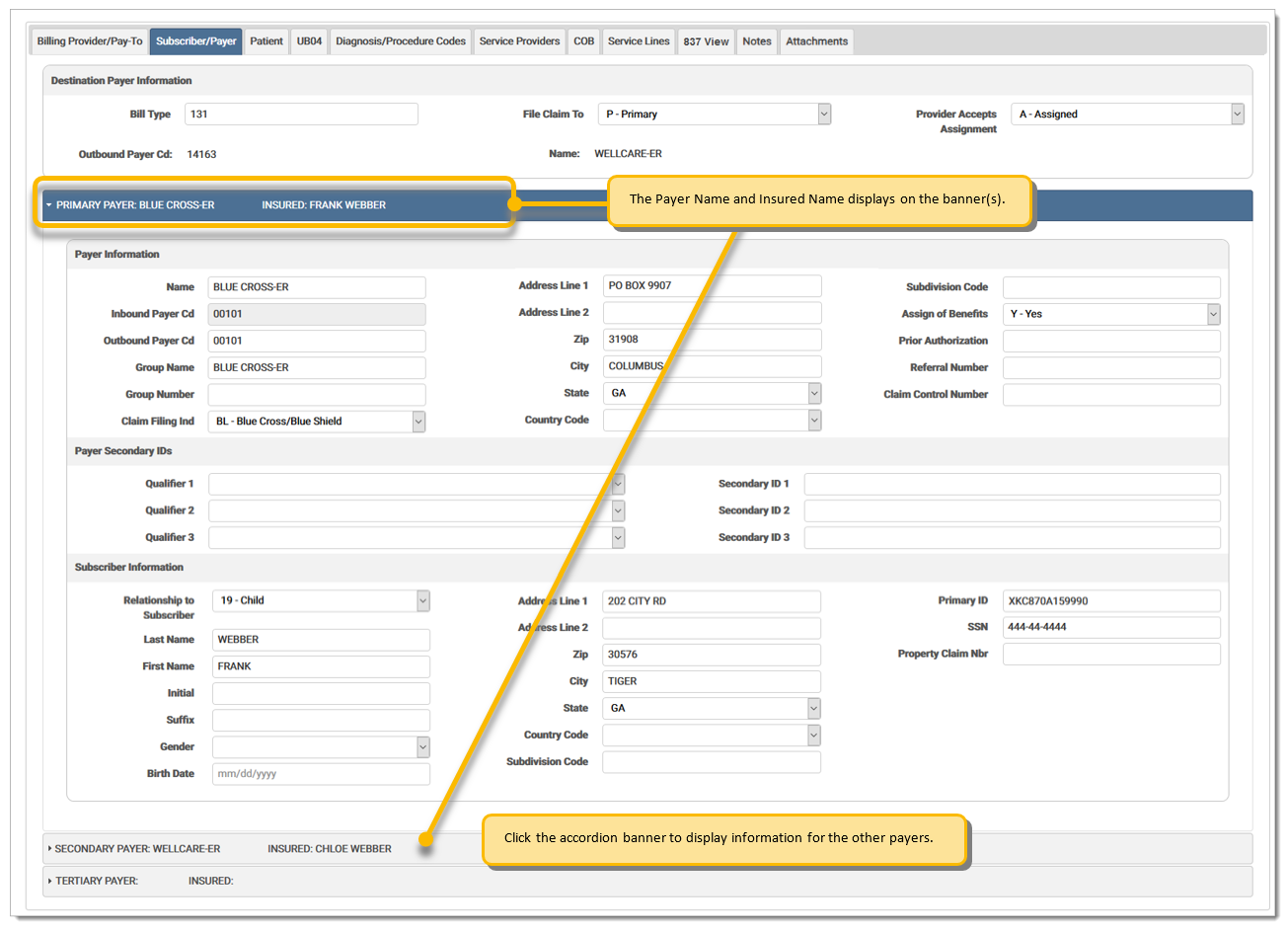
The Subscriber/Payer tab for institutional claims displays information about the insurer and insured person. This screen includes Primary, Secondary, and Tertiary options for the following:
Payer Information: Information about the payer or insurer, including insurance plan details and address.
Subscriber Information: Information about insured person, such as address.
A claim must have at least one payer. If all payers are deleted, an error message displays. Please select a payer from the Search option. The Search option allows the user to select a new payer. Users may manually enter information in this screen, or select a payer if one is already created in the Payer section.
On ASC and GSC claims, if the subscriber names (first and last) are the same for both the primary and secondary payer, the primary subscriber Gender and DOB is automatically populated into the secondary payer subscriber fields. If the name is not an exact match, it is not copied.
The Subscriber/Payer fields are defined by section below:
Code indicating the specific type of bill (inpatient, outpatient, adjustments, voids, etc.).
Provider Accepts AssignmentProvider Accepts Assignment
Code indicating whether the provider accepts assignment. Options are:
| A | Assigned |
| B | Clinical Lab Services Only |
| C | Not Assigned |
Select Primary, Secondary, or Tertiary from the drop-down menu.
Outbound Payer CodeOutbound Payer Code
Code number identifying the payer organization from which the provider might expect some payment from the bill.
Name identifying the payer organization from which the provider might expect some payment for the bill.
Select the desired payer from the drop-down menu. The payer information populates in the fields.
Name identifying the payer organization from which the provider might expect some payment for the bill.
Inbound Payer CodeInbound Payer Code
The payer code on the incoming claim file.
Outbound Payer CodeOutbound Payer Code
The payer code on the outbound claim file. This may or may not be the same as the inbound payer code. In cases where mapping needs to occur, RCM will use the inbound payer code to identify the payer specific actions that are needed. In some cases, this can result in a different payer code on the outbound claim.
The group name of the insurer.
The group number of the insurer.
Claim Filing IndicatorClaim Filing Indicator
Code indicating what type of insurance the covered person has available. This field is required prior to the mandated use of a National Plan ID. Options are:
| 11 | Other Non-Federal Programs |
| 12 | Preferred Provider Organization (PPO) |
| 13 | Point of Service (POS) |
| 14 | Exclusive Provider Organization (EPO) |
| 15 | Indemnity Insurance |
| 16 | Health Maintenance Organization (HMO) Medicare Risk |
| 17 | Dental Maintenance Organization |
| AM | Automobile Medical |
| BL | Blue Cross/Blue Shield |
| CH | Champus |
| CI | Commercial Insurance Company |
| DS | Disability |
| HM | HMO |
| LM | Liability Medical |
| MA | Medicare A (Inst Only) |
| MB | Medicare B |
| MC | Medicaid |
| OF | Other Federal Program (Use when submitting Medicare Part D claims) |
| TV | Title V |
| VA | Veterans Affairs Plan |
| WC | Workers' Compensation Health Plan |
| ZZ | Mutually Defined - Unknown |
Address of the subscriber.
Postal zip code of the subscriber. When a user enters a zip code in a zip code field and clicks tab to move to the next field, the city and state fields are automatically generated based on data received from the USPS. Note: This replaces any data already entered in the city/state fields.
City of the subscriber.
State of the subscriber.
Code indicating the geographic location.
Subdivision CodeSubdivision Code
Code identifying the country subdivision.
Assignment of BenefitsAssignment of Benefits
A code showing whether the provider has a signed form authorizing the third party payer to pay the provider. Options are:
| Y | Yes, benefits assigned |
| N | No, benefits not assigned |
| W | Not Applicable |
Prior AuthorizationPrior Authorization
Code number identifying the primary payer organization from which the provider might expect some payment for the bill.
Referral NumberReferral Number
A number or other indicator that designates that the treatment covered by this bill has been authorized by the payer. Required where services on the claim were pre-authorized or where a referral is involved. Generally, the pre-authorization/referral numbers are those numbers assigned by the payer/UMO to authorize a service prior to its being performed. The UMO is generally the entity empowered to make a decision regarding the outcome of a health services review or the owner of information.
Claim Control NumberClaim Control Number
The control number assigned to the original bill by the payer or the payer’s intermediary.
Code qualifying the reference identification. Options are:
| 2U | Payer Identification Number |
| EI | Employer's Identification Number (this must be a string of exactly nine numbers with no separators - e.g., 001122333) |
| FY | Claim Office Number |
| NF | National Associates of Insurance Commissioners (NAIC) Code |
Payer additional identifier.
Relationship to SubscriberRelationship to Subscriber
Select the patient's relationship to the subscriber from the drop-down menu. When manually keying a claim, the user is able to save a patient relationship code for each subscriber for each payer. The patient relationship code on an imported claim displays as it appears on the file. On an imported claim, when the patient is not the subscriber for the destination payer and the SBR02 is blank for the destination payer, the field is blank on this screen. Options are:
| 01 | Spouse |
| 18 | Self |
| 19 | Child |
| 20 | Employee |
| 21 | Unknown |
| 39 | Organ Donor |
| 40 | Cadaver Donor |
| 53 | Life Partner |
| G8 | Other Relationship |
The last name of the insured individual or subscriber to the coverage.
The first name of the insured individual or subscriber to the coverage.
The middle initial of the person insured individual or subscriber to the coverage.
The suffix of the insured individual or subscriber to the coverage.
Gender of the subscriber to the indicated coverage or policy.
Date of birth of the subscriber to the indicated coverage or policy.
Primary identification number of the subscriber to the coverage.
The Social Security Number of the subscriber to the coverage.
Address of the payer.
Postal zip code of the payer. When a user enters a zip code in a zip code field and clicks tab to move to the next field, the city and state fields are automatically generated based on data received from the USPS. Note: This replaces any data already entered in the city/state fields.
City of the payer.
State of the payer.
Code indicating the geographic location.
Subdivision CodeSubdivision Code
Code identifying the country subdivision.
Property Claim NumberProperty Claim Number
Identification number for property casualty claim associated with the services identified on the bill.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.