

Users may view professional claims, which contains 11 data entry tabs.
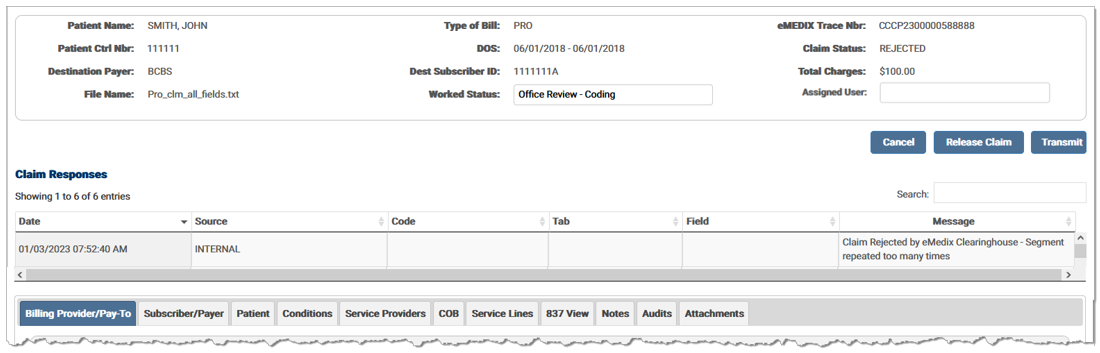
The Billing Provider/Pay-To tab contains Billing and Pay-To claim data.
The Subscriber/Payer tab contains information about the insurer and insured person. It includes Primary, Secondary, and Tertiary options for the Payer and the Subscriber. A claim must have at least one payer and subscriber.
The Patient tab contains patient specific information, including demographic information.
The Conditions tab contains all the data that identifies the condition of the patient. Options are located within accordion banners. Click the desired banner and enter any information needed for the claim.
The Service Providers tab contains information regarding the various claim level service providers. Enter any information on the Rendering Provider, Referring Provider, Additional Referring Provider Information, Supervising Provider, and/or Service Facility Provider.
The claim level Coordination of Benefits information is entered in the COB tab. This information is used to indicate the total monetary amount reported.
The Service Lines tab contains the procedures and charges for the claim or encounter.
The 837 View tab contains the current claim data in an ANSI format.
The Audits tab contains a record of changes made to the claim.
The Notes tab contains any notes associated with the claim and allows users to attach notes to the claim.
The Attachments tab contains information regarding attachments for the claim. Users can upload and submit attachments to payers. This tab is only visible if the payer accepts electronic or print/mail attachments.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.