

The Billing Provider/Pay-To Information section for professional claims displays information about providers. Typically, this information is supplied by your Information System.
The two main sections of this screen are:
Billing Provider: The original entity that submitted the claim/encounter to the destination payer.
Pay-To Provider: This information is required if the Pay-To provider is a different entity from the Billing provider.
Add any Secondary IDs as needed.
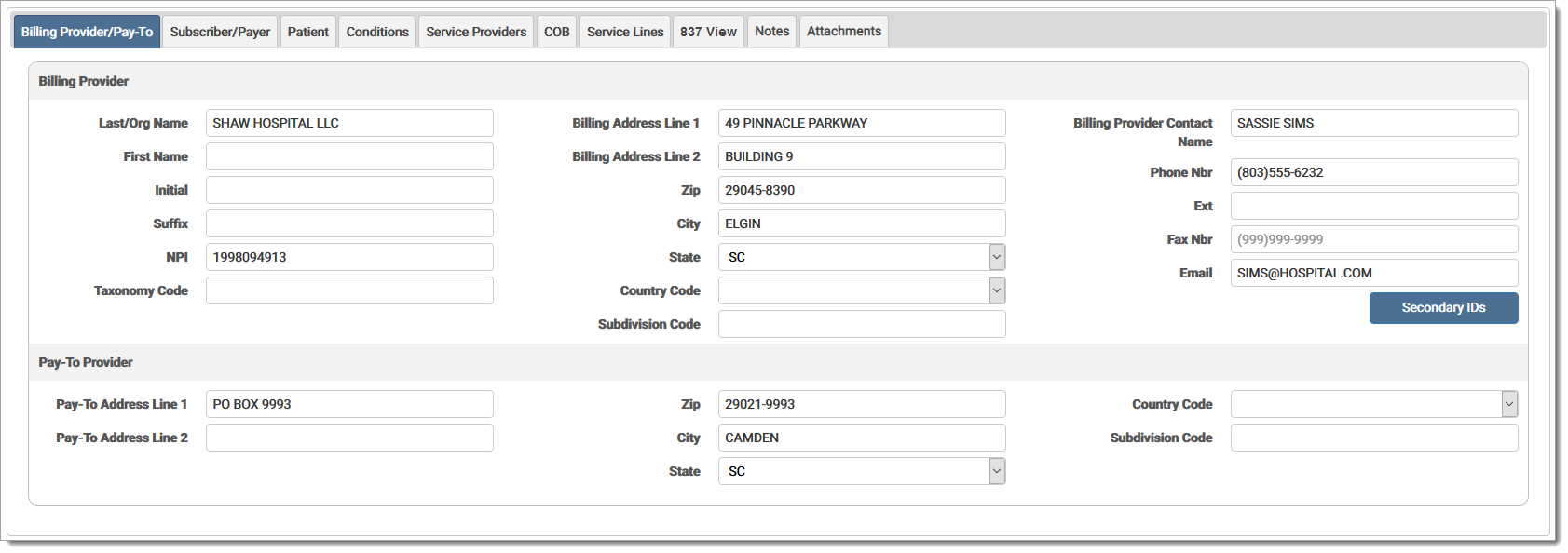
The Billing Provider/Pay-To fields are defined by section below:
Billing Provider Information: The original entity that submitted the electronic claim/encounter to the destination payer.
Billing ProviderBilling Provider
Select billing provider or billing entity from drop-down menu, if needed.
The name of the original entity that submitted the electronic claims/encounter to the destination payer. If the billing provider is a person, enter the last name, otherwise enter the organization name.
First name of the billing provider or billing entity.
The middle initial of the billing provider or billing entity.
Suffix, including generation, for the name of the provider or billing entity submitting the claim (e.g. Jr., III).
The principal identification number of the billing provider (often a provider has more than one number).
Code designating the provider type, classification, and specialization of the billing provider for this claim. The billing provider entity may be a health care provider, a billing service, or some other representation of the provider. The taxonomy can be different for the same provider on different claims.
The Health Care Provider Taxonomy Code list (provider specialty code) is available on the Washington Publishing Company web site: http://www.wpc-edi.com.
Billing Address Lines 1 & 2Billing Address Lines 1 & 2
Address of the billing provider or entity.
Postal zip code for the billing provider or entity. When a user enters a zip code in a zip code field and clicks tab to move to the next field, the city and state fields are automatically generated based on data received from the USPS. **This is a required field for Canada and the US.
Note: This replaces any data already entered in the city/state fields.
City of the billing provider or entity.
State of the billing provider or entity.
Code indicating the geographic location.
Subdivision CodeSubdivision Code
Code identifying the country subdivision.
Billing Provider Contact NameBilling Provider Contact Name
Enter the name of the person to contact regarding the transaction.
Telephone number of the contact person.
Telephone extension of the contact person.
Fax number of the contact person.
Email address of the contact person.
Secondary IDs: Add any secondary IDs as needed.
Qualifer: The type of ID number used in the billing provider's Secondary ID field. Options include:
| 0B | State License Number |
| 1G | Provider UPIN Number |
| EI | Employer’s ID Number |
| G2 | Provider Commercial Number |
| LU | Location Number |
| SY | Social Security Number (the Social Security Number may not be used for Medicare) |
ID: The secondary identification number of the billing provider.
Pay-To Provider Information: This information is required if the Pay-To Provider is a different entity from the Billing Provider.
Pay-To ProviderPay-To Provider
Select the Pay-To Provider from the drop-down menu if it is a different entity from the billing provider or billing entity.
Pay-To Address Lines 1 & 2Pay-To Address Lines 1 & 2
Address of the provider to receive payment.
Postal zip code of the entity to receive payment. When a user enters a zip code in a zip code field and clicks tab to move to the next field, the city and state fields are automatically generated based on data received from the USPS. Note: This replaces any data already entered in the city/state fields.
City of the provider to receive payment.
State of the provider to receive payment.
Code indicating the geographic location.
Subdivision CodeSubdivision Code
Code identifying the country subdivision.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.