

The Adjudication is used to convey service line adjudication information for coordination of benefits between the initial payers of a health care claim and all subsequent payers. This information is required when the claim has been previously adjudicated by the payer and this service line has payments and/or adjustments applied to it.
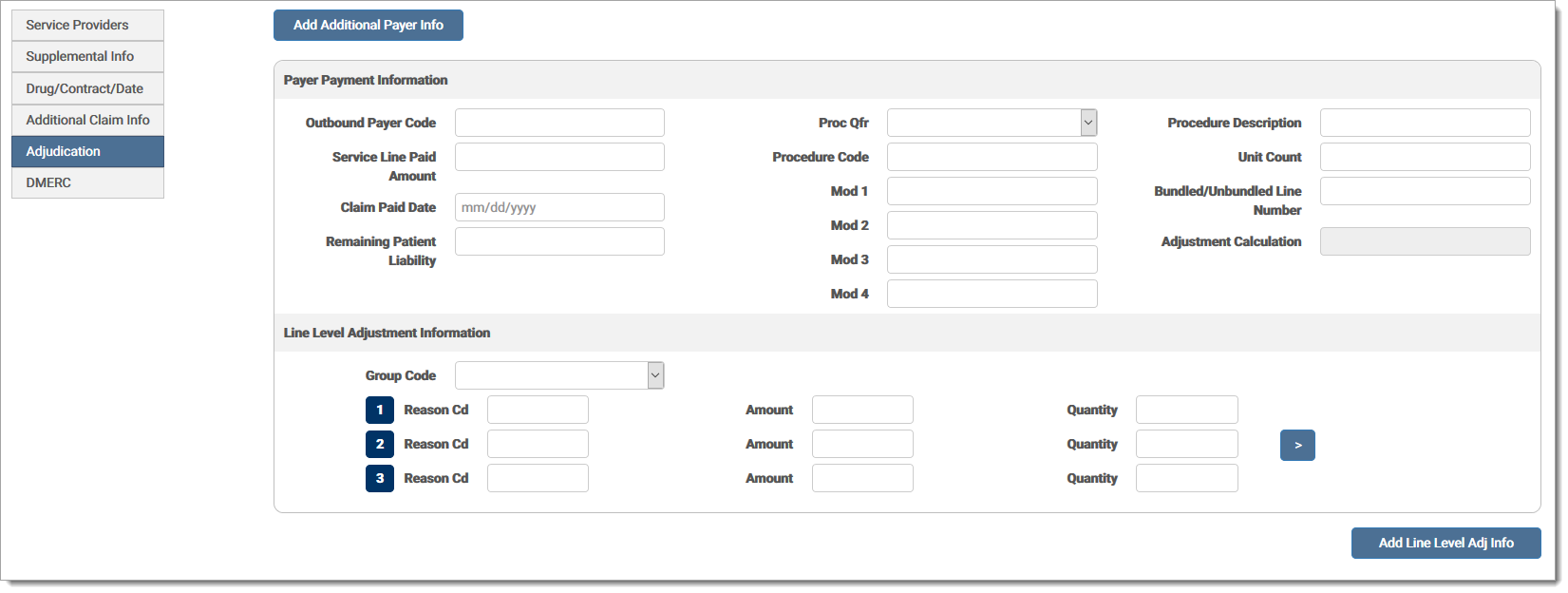
The Adjudication fields are defined by section below:
Payer Payment Information: This section provides information relating to the payer responsible for the reimbursement.
Outbound Payer CodeOutbound Payer Code
Other payer primary identifier.
Service Line Paid AmountService Line Paid Amount
Amount paid by the indicated payer for a service line.
Claim Paid DateClaim Paid Date
Adjudication or payment date.
Remaining Patient Liability Remaining Patient Liability
In the judgment of the provider, the amount that remained to be paid after adjudication by the other payer.
Procedure QualifierProcedure Qualifier
Product or service ID qualifier. Options are:
| ER | Jurisdiction Specific Procedure and Supply Codes |
| HC | Health Care Financing Administration Common Procedural Coding System (HCPCS) Codes |
| IV | Home Infusion EDI Coalition (HIEC) Product/Service Codes |
| WK | Advanced Billing Concepts (ABC) Codes |
Identifying number for a product or service.
Identifies special circumstances related to the performance of the service, as defined by trading partners.
Procedure DescriptionProcedure Description
Procedure code description.
Paid service unit count.
Bundled/Unbundled Line NumberBundled/Unbundled Line Number
Number assigned for differentiation within a transaction set. Required when payer bundled this service line. If not required, do not send.
Adjustment Calculation Adjustment Calculation
This field automatically calculates the line level adjustments and cannot be edited. It displays the sum of the total adjustments plus the payer paid amount, allowing the user to view if the adjustments balance.
Add Additional Payer InfoAdd Additional Payer Info (button)
Click to add additional payer information. Up to three (3) additional payers can be added.
Line Adjustment Information: This section provides adjustment reason codes and amounts as needed for an entire claim or for a particular service within the claim being paid. Adjustment information is intended to help the provider balance the remittance information. Adjustment amounts should fully explain the difference between submitted charges and the amount paid.
Claim adjustment group code. Options are:
| CO | Contractual Obligations |
| CR | Corrections and Reversals |
| OA | Other Adjustments |
| PI | Payer Initiated Reductions |
| PR | Patient Responsibility |
Claim adjustment reason code. First three (3) are shown, may add three (3) more.
Claim adjustment amount.
Claim adjustment quantity.
Add Line Level Adjustment InfoAdd Line Level Adjustment Info (button)
Click to add additional line level adjustment information. Up to five (5) adjustments can be added.
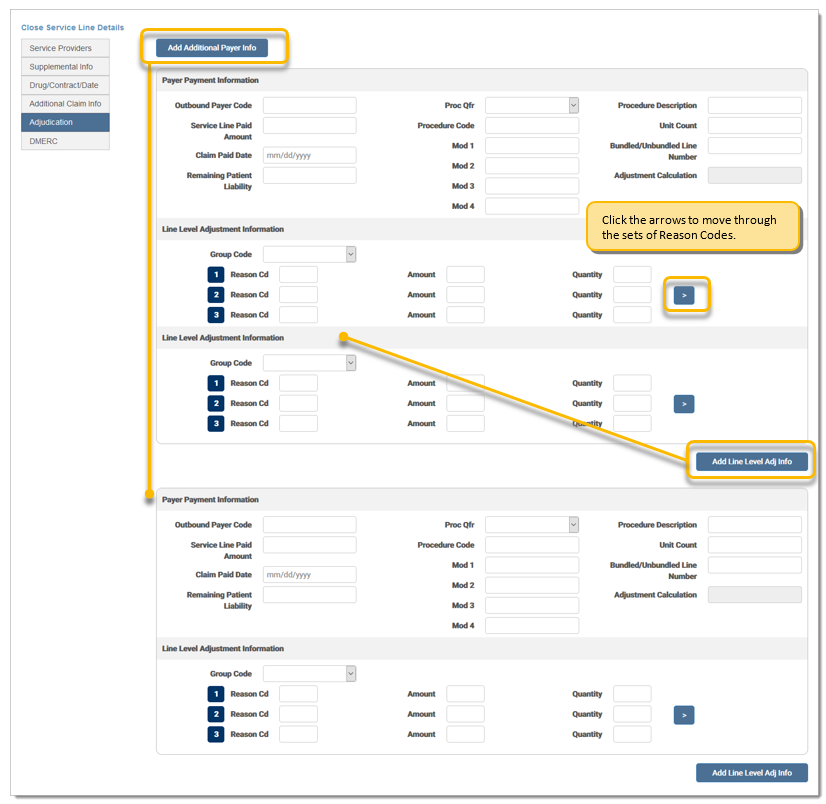
Line Level Adjudication screen options:
The user is able to add up to 15 sets of payer information, one at a time, by clicking the Add Additional Payer Info button. When the user clicks Add Additional Payer, a new payer payment and one line level adjustment section appears at the bottom of the screen.
The user is able to move through the six (6) sets of line level adjustment groups in the same box, three at a time by clicking the arrow on the right side of the section. The sets are numbered 1-6, allowing the user to easily view the set in which they are currently entering data. The user is able to arrow to sets 4-6 and then back to 1-3.
The user is able to add up to five (5) sets of line level adjudication information by clicking on the Add Line Level Adj Info button at the bottom left of the last line level set.
Each Payer Payment Information section includes a sub-group of the line level adjudication section.
Any blank records are removed once a user saves the claim.
eMEDIX Online | ©copyright 2025 CompuGroup Medical, Inc. All rights reserved.